Imagine there was a virtual copy of your body out there – a sort of clone, but in the digital world. And imagine that this clone encapsulated your full medical record: age, height, weight, pre-existing conditions, pulse, organ activity, cholesterol level, genetic predispositions and more. That’s the idea behind digital twins. They convert patients’ medical data into mathematical formulas which are then fed into AI algorithms and computer programs. They work in real-time and run not just on the medical data of the patient being treated, but also on the data generated by all other digital twins.
The goal is for doctors to use these virtual models to make predictions and deliver personalized healthcare. For instance, doctors could use a patient’s digital twin to detect a hidden cancer, test out various treatment protocols, observe the corresponding responses and select the best protocol for that particular individual.
Scientists believe that digital twins stand to revolutionize the practice of healthcare and take much of the mystery out of how to keep patients well. Digital twins have already been (or are in the process of being) developed for specific organs; one for the entire human body could be ready within 15 years. But behind this technological prowess lie several ethical questions, such as how exactly the virtual clones will be used and how patients’ personal data will be protected – especially if the twins are developed by the private sector.
Digitized objects
Digital twins have potential beyond the field of healthcare – virtual replicas have already been made of an array of objects, from engines and machines to entire cities. Engineers use these 3D computer models to predict the behavior of objects by conceptualizing the relationship between the physical and virtual worlds. In other words, a digital twin is a digitized version of a real-life object. “These models have shown to be capable of effectively replicating an object’s entire life cycle, from its production and use through its demolition or recycling,” says Frédéric Kaplan, head of EPFL’s Digital Humanities Laboratory.
When used in healthcare applications, digital twins are computer models of patients developed from their full medical records. “In theory, doctors will be able to use the models to adjust treatments to the specific characteristics of each patient. Many treatments today are designed for an ‘average patient’ but aren’t necessarily appropriate for distinct individuals,” says Kaplan.
Data at the heart of healthcare
In addition to allowing doctors to prescribe personalized, pre-tested treatments, digital twins offer a number of other advantages. They reduce the likelihood of errors in treatment and indicate exactly how effective a given treatment will be. “Digital twins can cut healthcare costs because they let doctors detect drug intolerances ahead of time and spot diseases before they reach the chronic stage. They can also reduce treatment errors, which are the third-leading cause of death worldwide after cancer and cardiovascular disease. All this implies considerable cost savings, says Adrian Ionescu, head of EPFL’s Nanoelectronic Devices Laboratory. One important challenge to have a Digital twin trusted and accurate is the quality of the data used to support to build them, which means the sensor hardware that should capture dynamic fingerprints of disease onset and progression in an accurate way.”
The AI algorithms used to create digital twins can also generate new data based on existing datasets. That means the algorithms will be able to fabricate virtual patients. One day, panels of such AI-born patients could replace the humans used to test new drugs and run clinical trials. This method already has a name: in silico testing. What’s more, digital twins can give indications about a patient’s family members based on the patient’s own medical history. That could be useful in detecting genetic disorders. “There are huge benefits to be had in analyzing such data, especially for new device development and for helping patients more effectively,” says Harald Studer, CEO of Optimo Medical, a firm based in Biel/Bienne which has developed a digital twin of the human eye.
According to Samia Hurst, a bioethics professor at the University of Geneva, digital twins could herald the end of animal testing. “If scientists could work on a computer model of a mouse’s body, for instance, they wouldn’t need to conduct experiments on living animals. They could run in silico simulations on virtual ones,” she says.
A natural next step
Are doctors really ready to embrace digital twins, given that many of them – as well as their patients – are even distrustful of electronic medical files? Both types of technology meet a real need, even if some segments of the healthcare industry are reticent. “Switzerland is far behind other countries when it comes to medical data,” says Jean Gabriel Jeannot, a general practitioner in Neuchatel. “But the truth is, treatments are becoming increasingly complicated and more patients are suffering from a chronic disease or a combination of diseases. These patients often have to see several specialists, and today there is no single shared network for communicating information among different practitioners. And we can’t permit ourselves to give patients care and diagnoses that are not based on electronically stored information. Digital twins, as a natural extension of electronic medical files, could help resolve that problem. We just need to see if doctors are willing to adopt the technology.” However, Jeannot thinks that patients themselves will end up driving the change. “If they want the technology, doctors will have no choice but to use it,” he says.
Switzerland is far behind other countries when it comes to medical data”
Twin eyes and hearts
While a full-body digital twin is still a ways off, some companies and public-sector research institutes have already created twins of specific organs. The French National Institute for Research in Digital Science and Technology (INRIA) and Dassault Systèmes have each developed a virtual replica of the human heart, Optimo Medical has its digital eye, and ExactCure (a startup based in Nice) offers a drug-testing application based on digital-twin technology. INRIA’s model heart is intended to help doctors design therapies for patients suffering from heart failure and to assist with intervention for ventricular tachycardia. INRIA scientist and coordinator of SimCardioTest, a European project that aims to create a digital twin for cardiac therapies, Maxime Sermesant explains: “With our system, cardiologists can generate a digital twin of a patient’s heart in around 30 minutes based on the results of a CT scan. And our system can save cardiologists a considerable amount of time, since they can test their p intervention on a digital twin beforehand. They’ll know exactly what to do once they get into the operating room.”
Optimo Medical’s digital twin is designed to facilitate cataract surgery. To create the twin, an ophthalmologist takes measurements of a patient’s eye and enters them into a computer program. According to Harald Studer: “Surgeons can adapt their procedures to each patient by testing them first on the model. The actual operations aren’t performed until the procedure has been programmed correctly and run on the digital twin. This nearly eliminates the risk of making an incorrect move.”
Dassault Systèmes has set a new goal of creating digital twins of organs and the human body, among others. The group’s researchers have already developed a digital twin of cancer cells and the heart. They are engaged in a brain twin programme and have incubated in their laboratory a digital version of the foot and ankle, comprising a complete reconstruction of the bones, joints, tendons, ligaments and soft tissue. “These types of models are always created in response to a specific need or problem to resolve. The one of the brain will be used to help patients who are resistant to epilepsy drugs, for example,” says Patrick Johnson, SrVP Corporate Science & Research at Dassault Systèmes.
This nearly eliminates the risk of making an incorrect move”
Waiting for funding
Some scientists are still doubtful about the prospects for a full-body digital twin – but not EPFL’s Ionescu. “We can already collect data on our genomes and metabolism, and evaluate how environmental factors like air pollution, diet and stress levels affect us. We’ve overcome the first hurdle, which was to find a way to collect and process all that high-quality data with advanced micro and nanotechnology. We can also find certain features in the collected data with current machine learning algorithms. The next challenge will be to develop intelligent methods for interpreting them, which we’ll do with artificial intelligence, while the final decision and action will remain with the human factor” he says.
One obstacle to the wider adoption of digital twins in healthcare is the broad range of skills they require along with a hefty amount of funding. That’s also why many public-sector institutions like EPFL don’t have specific R&D programs for digital twins, and why much of the development work is being done by the private sector. “To build a digital twin, you have to draw on knowledge from a host of different disciplines, from engineering and sensor design to machine learning and medicine. All the technology has already been invented, we just need to bring it all together. And for that, we need strong political will,” says Ionescu.
Dr. Jeannot points to how things are currently out in the field. He believes that doctors and other practitioners are not yet ready to work with virtual clones. “Digital twins will struggle to gain acceptance unless healthcare professionals get behind them. Even today, some doctors still use fax machines. Technology adoption in this industry will undoubtedly have to be driven by patients,” he says.
The ambiguities of the private sector
While it may sound appealing to have a digital twin undergo medical examinations for you, there are still many question marks surrounding this approach. Digital twins work by amassing reams of medical data to feed AI algorithms and make sure they run properly; the more data they have, the more accurate their predictions. For now, companies and hospitals developing digital twins use patient data only after getting their express written consent. But less scrupulous developers could take advantage of leaks in IT security systems to source data directly on the internet.
Public-sector entities have an additional handicap – a lack of funding for digital-twin technology. Most medical data for digital twins comes from hospitals, but it’s not clear how long they’ll be able to compete with the private sector. “Public-sector entities could very well decide to partner up with businesses to develop and market digital twins,” says Valérie Junod, a lawyer and a law professor at the University of Lausanne. But in that case, what would happen to our medical data once they’re in the hands of the private sector? Would they remain secure? And what would the consequences be if digital twins are developed not in the interests of the public good, but for a profit motive?
Public-sector entities could very well decide to partner up with businesses”
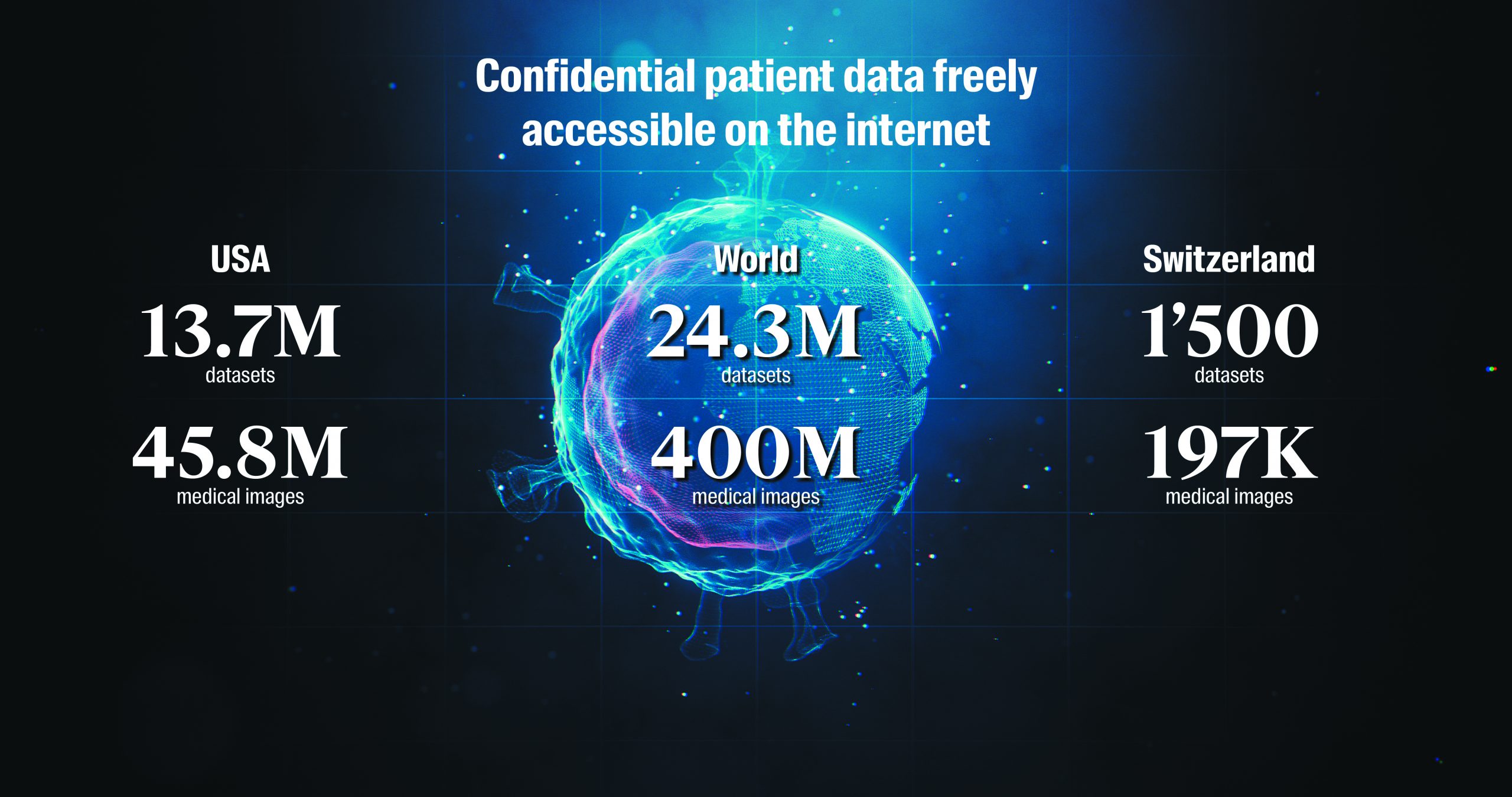
Données confidentielles sur les patients librement accessibles sur Internet - Copyright Greenbone Networks GmbH, 2019 © Istock & EPFL MCV
Thousands of images online
Greenbone, an IT security company based in Germany, has examined the specific issue of medical data security. As part of a study it conducted in 2019, the firm was able to access thousands of medical images and other kinds of medical data online from open-access platforms. And it found nearly 400 million medical images around the world that were available online or easily downloadable. The figures for the US were 45.8 million medical images and 13.7 million datasets; for Switzerland, 197,000 medical images and 1,500 datasets. According to Elmar Geese, Greenbone COO: “Today’s personal-data-protection laws and systems are inadequate. And digital twins pose an additional threat since they require huge amounts of data to function. Creating a digital twin entails collecting, analyzing and storing large sets of sensitive data. Many companies and scientists are focusing on the technological aspects and not paying enough attention to the data protection challenges. Some of them use cloud-based storage systems owned by the Big Four tech firms” – Alphabet, Amazon, Facebook and Apple – “since they’re cheap and easy to use. The catch is that they lose control of their data.”
The more data that are collected, the bigger the risk of a leak and the harder it is to keep the data anonymized. For Dr. Jeannot, a staunch advocate of technology in healthcare, digital twins could threaten doctor-patient confidentiality. “We’ll have to make 100% sure that patient data are – and will always be – secure and confidential. Otherwise digital twins will never take hold,” he says.
Ensuring data security
Johnson believes that the solution will come from a refined understanding of the offers: “We can consider the same issue with bank-account data. Banks, which are private-sector organizations, deployed major resources to make sure their customer data stay safe. It’ll be the same need in healthcare with digital twins. If a technology can’t guarantee full data protection, it won’t have any patients. That means companies will have to provide an offer secured cloud storage system that comply with the EU’s General Data Protection Regulation. Patients must obviously benefit from solutions that provide trust and full respect for their data.”
The laws in Switzerland are clear. With rare exceptions, patients must give their consent, specifying the nature of the uses to which their data will be put. “The laws won’t be scaled back in the medium term – on the contrary. They’ll probably be made even stiffer with additional restrictions on how personal data can be used and must be protected. And that’s despite the fact that scientists would like to see the restrictions eased so they can carry out their research more easily,” says Junod. She also points out that if patients agree to have their data used by a company based outside Switzerland, Swiss law doesn’t apply in the event of a dispute.
Political will
Ionescu acknowledges that digital twins carry an element of risk when it comes to storing medical data. “There are several possible solutions but none of them is perfect. The current thinking among scientists is that the data will be stored on local servers at each hospital, or perhaps in a national database. But we’re dealing with an international issue, and each country has its own policies. It would be good to have a pan-European medical database or maybe a ‘healthcare internet’ where data are stored and protected,” he says. One thing is sure though – the cloud as it exists today does not meet the security standards necessary for digital twins. If the EU or other governmental bodies decide to invest heavily in developing digital twins, they’ll be able to set their own rules for how medical data are collected, stored and used. The EU would probably apply the GDPR to the protection of patients and their medical data.
It would be good to have a pan-European medical database”
Who owns the code?
Another problem with the private-sector development of digital twins relates to the AI behind them. The businesses that own the code for the algorithms basically hold all the power over the technology. Experience has already shown that algorithms are not neutral and reflect programmers’ own cognitive biases. That means AI systems based on those algorithms are also somewhat biased. “Especially for healthcare applications, it’ll be crucial for scientists to be able to question and challenge the code. But if the code is owned by a business, how will they get access to it?” says Bertrand Kiefer, editor-in-chief of Revue Médicale Suisse. Today no one can argue with the choices made by AI algorithms or lodge complaints against their decisions. Machine learning is still a black box – and one that sometimes even the programmers and engineers themselves don’t fully understand and can’t explain.
Last but not least, there’s the issue of how reliable digital twins will be. No computer model of the human body can fully and faithfully represent all its natural mechanisms; the best these models can do is generate probabilities and statistics that practitioners must then interpret. Digital twins won’t provide any clear-cut answers but could be robust tools for prevention – albeit with their share of drawbacks.
Two-speed healthcare?
Digital twins will most certainly be expensive, meaning not everyone will be able to afford them. For now it’s hard to estimate the technology’s total development cost, but according to Ionescu, a parallel can be drawn with the resources needed for the first space missions. “Digital twins will be the next major technological advancement of the 21st century. But to make them happen, we need genuine political will backed by sizable funds,” he says. So if governments help finance the development work, does that mean digital twins will be made available to all citizens? Ionescu believes that the current approach will result in a two-speed healthcare system, at least in the beginning. “We have to start by using them somewhere. But for everyone to eventually have access, policymakers will need to make that a priority,” he adds.
Georg Starke, a PhD student at the Institute for Biomedical Ethics at the University of Basel, feels that digital twins will have to be affordable if they are to be adopted by the general public. “One way to turn them into low-cost, accessible solutions would be to implement them through a smartphone app. The app could record a user’s medical data and provide personalized recommendations to prevent the user from getting sick. However, such applications would require careful ethical oversight and regulation, for example to avoid exacerbating existing inequalities” he says. Johnson agrees: “Digital technology in general is intended to improve the lives of as many people as possible. If we want a system that people will actually use, it has to be digital, virtual, straightforward and intuitive. Complicated systems won’t survive.”
Digital technology in general is intended to improve the lives of as many people as possible”
The right not to know
The healthcare industry is no stranger to ethical questions. They often arise with regard to whether medical data should be sold for a profit, whether healthcare provision should be considered a market with supply, demand and economic gain, and how cost-benefit analyses should be conducted for R&D, for example. An exhaustive list of ethical questions for digital twins is hard to prepare since we don’t know the full extent of how they’ll be used. And because the twins will generate predictions about a patient’s health, doctors also need to consider issues related to patient information, and especially a patient’s right to know and not to know. “Digital twins throw questions like that into the spotlight – not just a patient’s right not to know, but also what should be done if a doctor stumbles across important information that wasn’t mentioned specifically in the consent form,” says Hurst. “How can a doctor comply with a patient’s wishes if the patient doesn’t even want to be told the information? And what if the information also concerned members of the patient’s family?” One idea Hurst has is to draw up a list of all the types of choices a patient would want to be receive -or not receive- medical information for.
A matter of semantics
Perhaps society’s fears about digital twins – and AI technology in general – are a bit overblown. After all, isn’t it basically just a matter of semantics? According to Johan Rochel, co-founder of ethix – a startup that studies ethical issues related to digital technologies – it’s important to use the right terms in order to play down worries that are probably unfounded. “Digital twins are nothing more than comprehensive medical files which are used to compare a patient’s data with those stored in databases. Advanced algorithms run simulations on the developments of one’s health’s conditions. The word ‘twin’ is merely a way to humanize the technology and tell a story based on the idea of a digital avatar. Databases and algorithms bear incredible premises for personalized health, but there is no requirement to tell a story about digital twins,” he says. Ionescu adds: “Digital twins will never replace actual practitioners. They’re just another tool in the toolkit.”
A clear path ahead
Scientists are optimistic about the potential for digital twins in healthcare, despite the fact that the human body is a complicated, multi-scale being with various ways of working and a myriad of connections among its organs. Businesses and researchers agree that model organs have already brought a lot to the field of medicine, and will only become more powerful and robust as time goes on.
The biggest challenge in getting digital twins adopted by the healthcare industry will be making sure that patient data are anonymized and protected. That will be an uphill battle, considering how much of our personal data are already held by businesses as a result of our social media posts and online purchases, as well as the increasingly popular DNA home-testing kits. But scientists and experts agree on one thing – we need to address the issue of medical data protection and use, as well as the ensuing ethical questions, now while the development work is still going on.
Digital twins may seem like an abstract concept, but they will likely be part of the medical landscape within a few years. And given all the fears and concerns they raise, the future may hold some interesting twists and turns – including some that even artificial intelligence wouldn’t have predicted. ■








